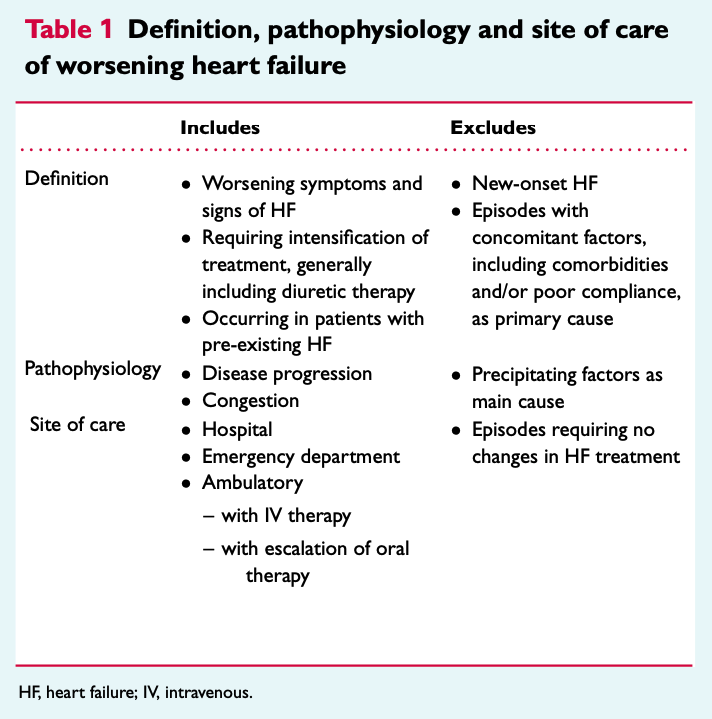
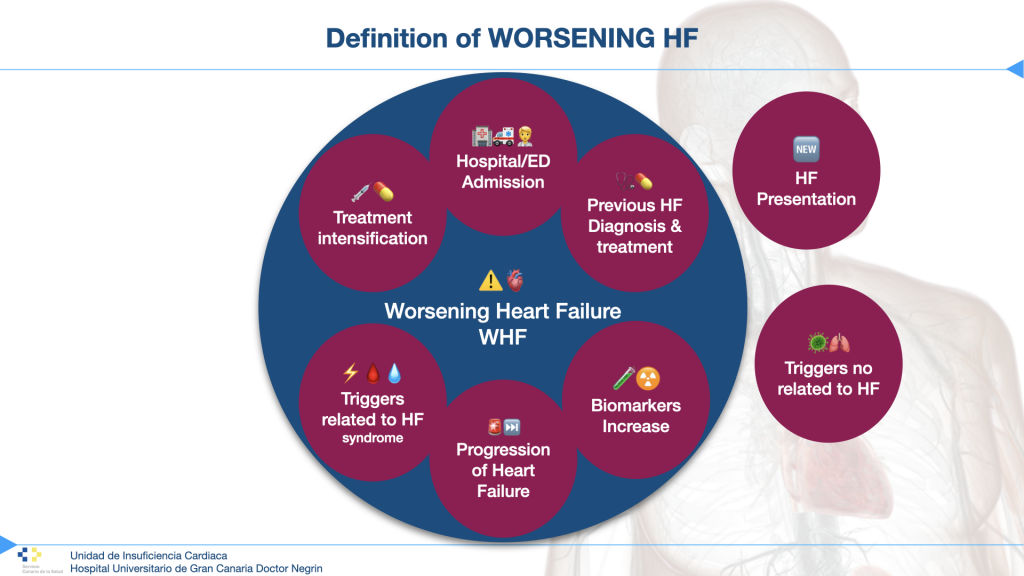
In the consensus about worsening heart failure from the HFA1, worsening heart failure may be confused with progression of heart failure. The definition narrows the group of patients who would potentially benefit from the new treatments for worsening heart failure.
Patients with worsening heart failure include patients with disease progression. It is important to identify patients with progression because they will benefit from more appropriate treatments for advanced heart failure. Those patients with worsening heart failure due to identifiable comorbidities cannot be excluded from the definition because some of them, such as atrial fibrillation, renal failure, or anemia, are closely related to heart failure syndrome. This is quite different from other circumstances that lead to decompensation, and that are common to other diseases, such as lack of adherence, dietary transgression, infections, etc.
In our series of patients admitted for heart failure, the main causes identified by clinicians are arrhythmias (mainly atrial fibrillation), anemia, renal failure, etc., and others not related to heart failure syndrome such as infections (mainly respiratory and urinary tract), lack of adherence, dietary transgression, etc. On the other hand, anemia can be part of heart failure syndrome or related to digestive bleeding, for example. The worsening of heart failure would have a broader spectrum than that described in the definition, which is more like the progression of heart failure, which is usually much less frequent in decompensation.
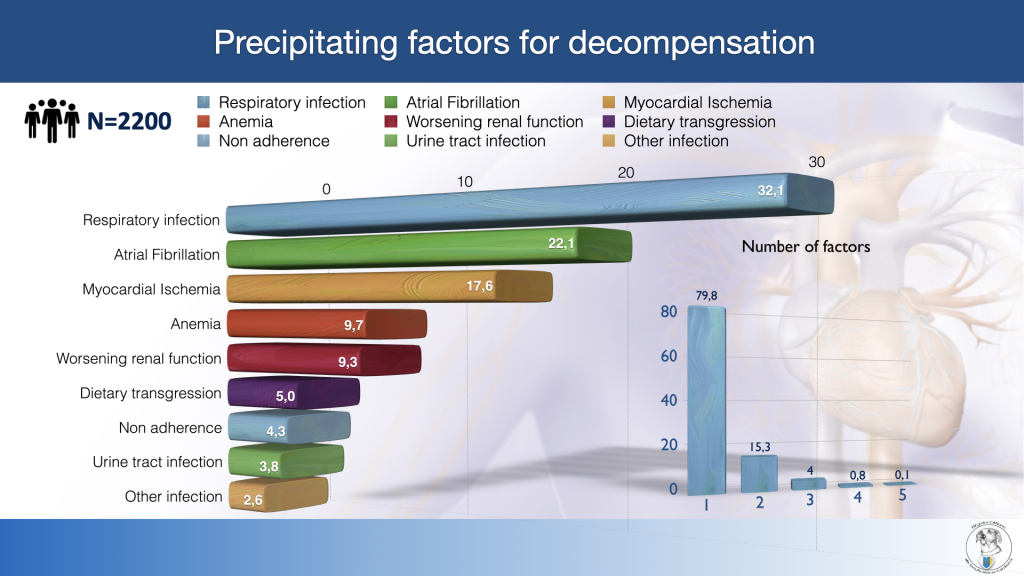
Precipitating factors are frequently associated to decompensation, and sometimes (20%) there more than one factor related. Some of them could be not related to heart failure syndrome, but other are related to the disease progression as well. So, these patients should not be excluded from the definition of worsening heart failure. Other way the definition will be very close to progression of HF, even regarding that HF trend is to progress with time.
The definition given in this statement seems to be close to the definition of progression. Those patients are a reduced group compared to those with worsening heart failure, regarding some precipitating factors that in some instances are part of the syndrome (progression of the atrial myopathy, mitral regurgitation, renal failure, …). Even those patients include in clinical trials about worsening heart failure like VICTORIA-HF2 doesn’t exclude patients with precipitating factors of decompensation, while others like SOLOIST-HF3 excluded patients with high-rate AF/flutter (>130 bpm), severe anemia, COPD exacerbation, or infection. Obviously, all of them excluded patients with recent acute coronary syndrome, pulmonary embolism, or cerebrovascular accident.
Regarding the success of these trials, their selection criteria should contribute to the definition as well. The key seems to be to make the difference between:
a) Intrinsic precipitating factors of decompensation related to heart failure (atrial fibrillation, MR progression, EF worsening, anemia, ventricular tachycardias, worsening renal failure, treatment intolerance…), from
b) Those factors related to extrinsic conditions (Infections, COPD exacerbations, non-adherence, financial toxicity, dietary changes, or acute events like myocardial infarction or pulmonary embolism…).
This is our proposal to differentiate progression from worsening:
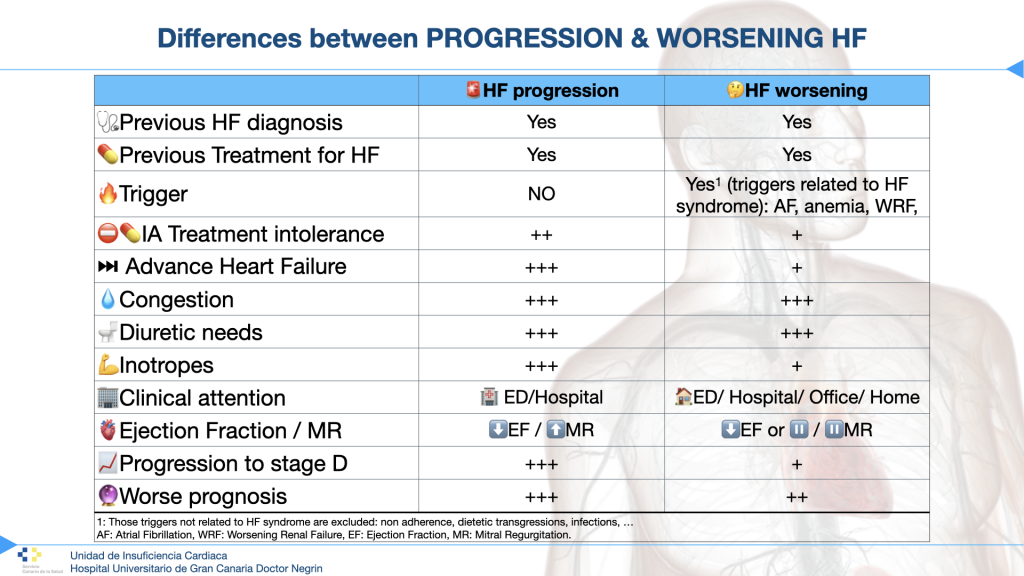
Identification of those patients with real progression of HF among those with worsening HF would be crucial in order to benefit from advance HF therapies.
Bibliography:
1. Metra M, Tomasoni D, Adamo M, et al. Worsening of chronic heart failure: definition, epidemiology, management and prevention. A clinical consensus statement by the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. Published online 2023. doi:10.1002/ejhf.2874
2. Armstrong PW, Pieske B, Anstrom KJ, et al. Vericiguat in Patients with Heart Failure and Reduced Ejection Fraction. New Engl J Med. 2020;382(20):1883-1893. doi:10.1056/nejmoa1915928
3. Bhatt DL, Szarek M, Steg PG, et al. Sotagliflozin in Patients with Diabetes and Recent Worsening Heart Failure. New Engl J Med. 2020;384(2):117-128. doi:10.1056/nejmoa2030183
