The new 2021 ESC guidelines on heart failure ( https://doi.org/10.1093/eurheartj/ehab368) have established a foundational treatment based on four sort of drugs, and a lot more of drugs, devices and interventions based on patient characteristics. So it could seems a little bit messy and confused for those physicians not familiarized with this syndrome, for example, regarding when to start the treatment or what drug come first.
About the first, when to start, there a wide opinion that it should be as soon as possible (ASAP) and that the changes should be implemented every 1-2 weeks to reach a complete titration in about three to six months.
With respect to the second comment, what come first, it is no so clear now because all drugs are at the same level. The election of drugs by the order in which its evidence has been added to the guides could be reasonable, but we should not forget that all the therapies that have come after showed a significant effect on top of the previous treatments. That is one of the reasons to remove the sequential approach.
Obviously the election of drugs will depend on the patient clinical status, recovery from decompensation, congestion, blood pressure, heart rate, renal function and ions levels,… But we should have a plan, with many alternatives as all good plans, regarding the obstacles that can emerge and taking in mind all the available options.
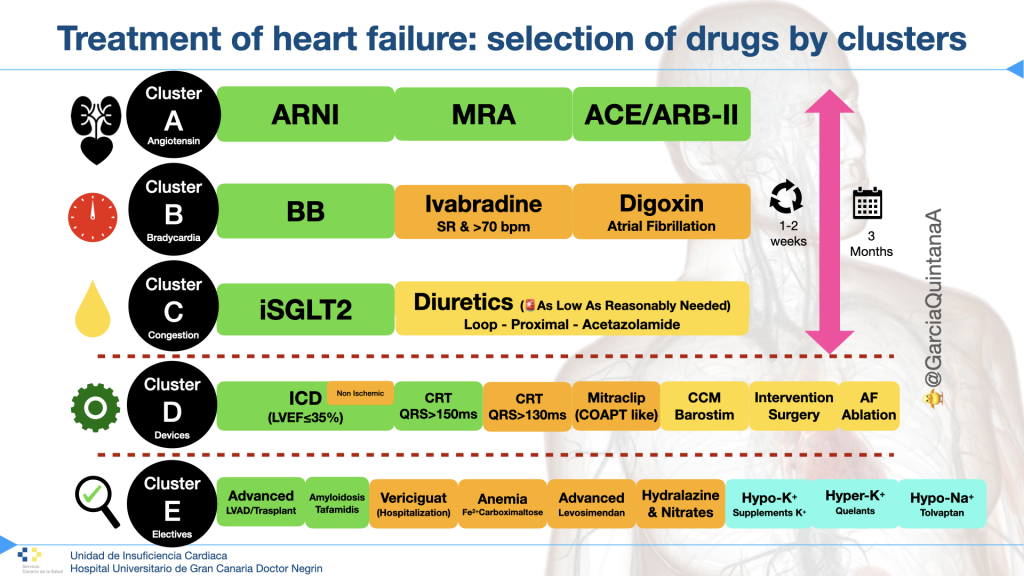
A classification of the therapies from the therapeutic arsenal could be appropriate to order them in our mind, and that is the reason of this simple proposal from A to E:
♥️A: Angiotensin-Renin-Aldosterone Inhibitors. This group is key and include several drugs with the common action on the Angiotension-renin-aldosterone system. Sacubitril/valsartan adds the beneficial effect of the inhibition of natriuretic peptides degradation.
⏱B: Betablockers and other bradycardia agents. BB have a well stablished evidence in sudden death reduction as well as in HF progression. Other agents tha promote bradycardia should be considered (ivabradine or digoxin) regarding the patients characteristics.
🚰C: Congestion modifiers and beyond. This group include iSGLT2 drugs with indication class I and with many other favorable effects beyond glucosuria. The diuretics should be use with the minimal dose to control congestion (🚨ALARN: as low as reasonable needed). Other extrarenal options to control congestion have not been considered here (Peritoneal dialysis, ultrafiltration, SCUF, …)
⚙️D: Devices and interventions. Devices are very important in terms of clinical improvement al prognosis. After the proven effects of remodeling of several drugs they have been delayed awaiting for the improvement of the LVEF. Nevertheless, in some cases with a extensive and diffuse transmural scar (by CMR for example), in whom this improvement is unlikeliy, ICD implantation with or without CRT could be anticipated.
🔎E: Electives treatments. These are the treatments applied to specific populations regarding their condition (amyloidosis and tafamidis) or clinical profile (worsening HF and vericiguat) and others to correct ionic disarragements.
Bibliography:
1. McDonagh, T. A. et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failureDeveloped by the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) With the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J ehab368 (2021) doi:10.1093/eurheartj/ehab368.
2. McDonald, M. et al. CCS/CHFS Heart Failure Guidelines Update: Defining a New Pharmacologic Standard of Care for Heart Failure With Reduced Ejection Fraction. Can J Cardiol 37, 531–546 (2021).
3. O’Meara, E. et al. CCS/CHFS Heart Failure Guidelines: Clinical Trial Update on Functional Mitral Regurgitation, SGLT2 Inhibitors, ARNI in HFpEF, and Tafamidis in Amyloidosis. Can J Cardiol 36, 159–169 (2020).
@GarciaQuintanaA